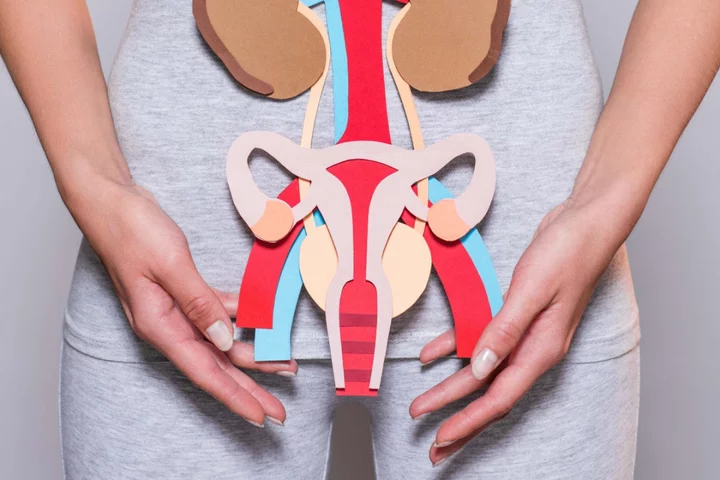
September is Gynaecological Cancer Awareness Month, which sees charities joining together to put the spotlight on the range of cancers that start in the female reproductive system.
There are five main types of gynaecological cancer – cervical, ovarian, vaginal, vulvar and uterine (or womb) – plus fallopian tube cancer, although this is very rare.
Around 22,000 women are diagnosed with a gynaecological cancer each year in the UK, of which 21 die every day, according to charity The Eve Appeal.
However, some of these cases are preventable, and with the right treatment, many gynaecological cancers have high survival rates.
Here, experts answer some key questions about the prevention and treatment of gynaecological cancers.
What are the symptoms of gynaecological cancers?
“The symptoms of gynaecological cancers can vary,” says gynaecologist Oudai Ali from New Victoria Hospital. “But some common signs to watch out for include abnormal vaginal bleeding, pelvic pain or discomfort, unusual vaginal discharge, new vulval lump or ulcer and changes in urinary or bowel habits.”
If you’ve noticed any of these signs, follow the ‘if in doubt, check it out’ rule, Ali says: “It’s crucial for patients to consult their GP if they experience any of these symptoms, as early detection can significantly improve treatment outcomes.”
Severe ongoing bloating and feeling full very quickly, unintentional weight loss and fatigue are also indications it’s a good idea to get things checked out.
Are regular screenings important for gynaecological health?
Routine screening programmes are not available for all types of gynaecological cancer. However, where they are available – such as cervical smear tests – attending screenings can be life-saving.
“Regular screenings, such as smear tests and HPV (human papillomavirus) tests, are vital for the early detection of cervical cancer and can prevent it at its pre-cancer stage,” says Ali. “Additionally, it’s important for individuals to discuss family history and risk factors with their healthcare provider to determine which screenings are appropriate.”
Research shows that cervical cancer risks are higher for people who don’t attend screenings.
“Cervical cancer risk is estimated to be 1.7% among women in the UK who don’t attend screenings,” says Mr Andrew Pooley, consultant gynaecologist at New Victoria Hospital. “Other risk factors are related to a higher exposure to HPV, the use of the contraceptive pill for over 10 years, or a weak immune system.”
Ali adds: “The age to start screening can vary depending on the type of cancer and a patient’s individual risk factors. Pap smears typically start around age 25.”
For cancers where there isn’t a national screening programme, your GP can refer you for blood tests and scans if you are concerned about symptoms.
Can gynaecological cancers be prevented?
While not all gynaecological cancers can be prevented, there are steps you can take that in some cases may help reduce your risk.
“Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and avoiding tobacco, can help,” Ali says. “The HPV vaccine is a powerful tool in preventing certain gynaecological cancers. It protects against several strains of HPV that can lead to cervical, vaginal, and vulvar cancers. It’s recommended for both boys and girls, ideally before they become sexually active, to provide the greatest protection.”
Some gynaecological cancers can have a hereditary component, too. “A family history of bowel, breast or ovarian cancer may increase the risk,” Ali explains, which is why it’s important to discuss family medical history at screenings. “They can assess the risk accurately and recommend appropriate screenings or genetic testing if necessary.”
This said, anyone can potentially get cancer, so getting any symptoms checked as soon as possible is always key.
What are the available treatment options for gynaecological cancers?
Treatment options vary depending on the type and stage (from one to four) of cancer.
“They may include surgery, chemotherapy, radiation therapy, hormone therapy, targeted therapy, or a combination of these treatments,” says Ali. “The choice of treatment is personalised to each patient’s specific diagnosis and medical history.”
Survival rates for the main five gynaecological cancers when diagnosed at stage one range from 75%-95% according to Cancer Research, which further highlights the importance of early detection.
New Victoria Hospital has launched its Community Champion Campaign, which will offer free scans and treatment to people across the UK for the sum of £125,000. To apply visit: newvictoria.co.uk/communitychampioninitiative.
Read MoreCharity boss speaks out over ‘traumatic’ encounter with royal aide
Ukraine war’s heaviest fight rages in east - follow live
Alzheimer’s: How and when to talk to someone about their memory loss
As Simon Cowell shares positive therapy experience, how can it help even if you aren’t in crisis?
Project launched to bust myth that cancer is a ‘white person’s disease’